We are here today to talk about all things pelvic pain.
What is pelvic pain? It can refer to any kind of pain between the belly button and the groin. It can affect folks of any gender but disproportionately affects folks assigned female at birth (AFAB), generally cisgender women and transmasculine folks. It’s estimated that pelvic pain affects up to 15% of women in the United States in their lifetimes, and 13-32% of women worldwide. I will be discussing chronic pelvic pain (CPP), which refers to pain in the vulvarvaginal area that lasts for six months or more, or is generally unresponsive to traditional treatments.
Diagnoses that fall under the CPP umbrella may include vulvodynia, vaginismus, endometriosis, pelvic inflammatory disease, prostatitis, interstitial cystitis, persistent urinary tract infections or bacterial vaginosis, spasm of various muscles in the pelvic floor area, or misfire of certain nerves in the area, among others. Sometimes no diagnosis or reason is provided at all, because doctors might not know the cause of the symptoms.
Creating Your Treatment Team
A crucial step in managing CPP is developing your treatment team.

People on your treatment team may include…
- OB/gynecologist
- Urogynecologist
- Urologist
- Gastroenterologist
- Pelvic Floor Physical Therapist
- Pelvic Pain Specialist
- Pain Specialist / Anesthesiologist
- Registered Dietitian
- Sex Therapist
- Hypnotherapist
Your team, much like your social circles, will develop over time. You will meet folks through other folks. Some will recommend you try new things and meet new people. Some people you will not get along with and not like and that is OK. Accept who you like and who you trust onto your team. Be open to new experiences.
Advocating For Yourself In Medical Settings
As folks with CPP diagnoses soon learn, one of the major parts of managing CPP is communication.
Whether it’s about what your symptoms are, where they occur, how they affect you, how you feel about them, when it started, what your relationship status is, how to find a doctor, what treatments to try, what you have tried and how it’s worked out for you thus far, what your sex life is like, which things are on or off limits now, a list of every trauma that has ever occurred to you, and every other diagnosis and symptom you might have ever had, or myriad other things, communication becomes a lifeline for folks managing CPP.
Something folks soon learn that they must deal with while managing a chronic health condition is advocating for themselves in a medical setting.
What does this look like for a person with CPP?
- Encouraging medical professionals to take your pain seriously
- Managing medical professionals’ lack of knowledge of human sexuality
- Managing medical professionals’ lack of exposure to sexual diversity
- Working through judgements from medical professionals whom we had hoped would be unbiased (they at times succumb to very “humanly” beliefs and attitudes based in fear and discrimination)
- Voicing your consent in at times invasive exams and treatments
- Navigating a system that tries to deny medical coverage, payment, and reimbursement for conditions that are complicated
- Dealing with a system that treats women’s health as lesser than
- Understanding that medical science is based on studies conducted on white men
Although doctors and other medical professionals are undeniably experts because of their schooling, training, and various expertises, please remember that you are the expert in your pain.
You know how it feels and where it happens. You know how it is affecting your life. You know what you will and will not welcome into your life and your body as viable treatments. You know what kinds of lifestyle adjustment recommendations you can accommodate.
A very important part of your journey will involve navigating the medical system and its various hoops and ladders and mazes and biases.
Before appointments, create a list of questions you have for your practitioner. Feel free to include any concerns you might have.
Listen to your gut. When you are at an appointment, take note of what your team is saying and how it is making you feel. I encourage you to reflect on this and to understand what this might mean for your treatment.

Understand, again, that healthcare practitioners are human beings who have also been raised in this sex-negative culture. Many have done “the work” to overcome biases, and are often still in the midst of doing “the work” (I know I’ll be doing it for probably all of my life). Some have not had the privilege yet for this undertaking.
I have heard practitioners tell folks with CPP myths around sexuality. “Sex is supposed to hurt,” “It’s not that bad, just deal with it,” “You’re just tight, men like that,” “You’re not having sex so don’t worry about it until then,” “You just haven’t met the right person yet,” “You’re being dramatic,” “Just have a few glasses of wine,” “It’s all in your head,” “You just need to relax,” “You’ll get used to it,” and maybe worst of all, some fall into the trap of just overlooking it and not talking about it at all.
First and foremost, you are valid. It’s ok to feel uncomfortable about the opinion of an expert. I do encourage you to seek other opinions, to seek referrals to doctors who “get it,” or to break up with a practitioner who is not benefiting you.
At Home Remedies
Your team will likely recommend medical treatments and interventions to treat or manage pain. Ask your doctors for recommendations and prescription medications. Here I will include recommendations for over-the-counter products that may provide some benefit to you. Please note: what works for some people doesn’t always work for everyone. Every body is different, and it’s recommended to do your own research and use your own judgment before using any kind of product. You know yourself best!
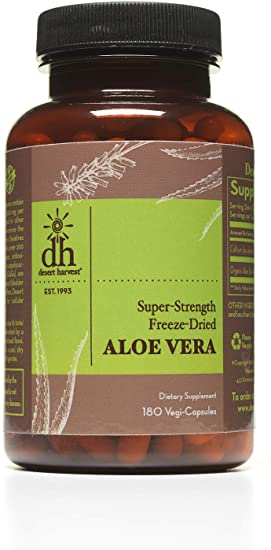
Desert Harvest makes a variety of aloe-based products that can help with lubrication and cell health/regeneration. Their aloe vera capsules are said to contribute to bladder health and decrease occurrence or symptoms of UTIs. They make aloe vera-based gels and lotions to lubricate the vulvavaginal area. They also make an aloe-based Releveum Gel (with 4% Lidocaine) that can help repair skin and alleviate topical pelvic pain.
Medicine Mama’s Apothecary makes various creams for vulvarvaginal health including their topical cream V Magic which “is an all-natural multi-purpose moisturizer specifically formulated to help soothe, protect and calm irritated tender vulvar skin.”

Lube becomes the loyal sidekick of a person managing CPP.
For folks who would like to try silicone-based lubricants, I would recommend Uberlube. Uberlube is compatible with condoms and is NOT compatible with silicone sex toys (check your dildos and dilators!).

For folks who would like to use a water-based lubricant or who need a lubricant to use with silicone sex toys and dilators, Good Clean Love makes safe and organic lubricants developed with women’s health and hygiene in mind.

Healing Body and Brain
Likewise, your treatment team will recommend medical interventions for managing and treating CPP. However, in addition to the aforementioned products to use for relief of symptoms, there are clinically proven methods to manage, alleviate, lighten, and work through symptoms of CPP.
First off, it’s highly recommended that folks with CPP bridge the medical gap between body and mind by seeking mental health counseling/therapy in addition to treatment by a physical doctor. Often in my work, this prompts the question, “Are you saying it’s all in my head?” To which I respond, “Your body’s processing of pain signals and your experience of physical pain happens in your brain, yes.” No, it’s not all in your head in the sense that you are choosing to do this to yourself. After all, you’re working to heal the pain! However, at the very least, having a space to discuss your CPP, and the life changes that accompany it, can be very beneficial. At the most, these professionals will suggest skills to manage and mitigate pain, suggest lifestyle changes to reduce stress, and relax the body, thus contributing to healing. Furthermore, counselors and therapists have more time to spend with you than medical doctors who are often allotted just fifteen minutes for an appointment. Over the course of this journey, it is likely that most of your time will be spent with a physical therapist or a counselor because they allot an hour or more for their appointment slots, and it’s encouraged that you attend weekly at the least. These are spaces for you to develop skills, get answers, and focus on yourself in an affirming and judgement-free environment.
Clinicians that have increased time to spend with you can help to explain the biology and science behind nociception, or the central nervous system’s responses to pain. Research shows that learning about pain can reduce your physical experiences of pain. Pain education has an effect not only on understanding how and why your body is doing what it does, but also can change your interpretation and experiences of physical pain. The research continues to come out on this subject. I highly recommend reading works by Lorimer Moseley, a leading pain scientist committed to retraining folks’ pain perceptions systems. Another scientist, John Sarno, is also worth checking out, who writes books about the interaction between brain and body in the experience of pain (The Mindbody Prescription), and is world-renowned on his ability to treat chronic back pain through pain education (Healing Back Pain).

Clinicians that have time to spend with you can also help you to better understand the cyclical nature between emotion and pain. We learned in school that pain is unidirectional – you cut your finger, your nerves notice the finger is hurt, and send the signal up to the brain. Done. Learning about pain informs us that this is not the case — the brain, central nervous system, and peripheral nervous system send signals throughout the pain experience, in both directions. Your emotional experience impacts your experience of pain perception and the resulting physiology of the pain. It can be as simple as anxious feelings that cause you to tense up, leading to muscle spasm that pinches a nerve. Or, it can be more nuanced, such as your upbringing in a sex-negative culture or religion influencing your brain’s interpretations of pain signals around the pelvic area. Either way, it is beneficial to work through this with a supportive, trained clinician.
Another thing recommended to folks managing CPP is Mindfulness-Based Stress Reduction (MBSR). The research as of late has exploded with the benefits of practicing MBSR. MBSR has been demonstrated over and over in research to have wide-reaching benefits to treat stress, anxiety, depression, chronic pain, and many other maladies. I highly recommend learning more about MBSR, and seeking a clinician trained in MBSR who can lead you through guided meditations. There are also apps for use on your phone, such as Calm and Headspace, that can train you in how to meditate.
Trained counselors, therapists, psychologists, and hypnotherapists can teach you these skills, as well as others that are currently emerging. Another related practice that you may learn is the emotional freedom technique, or EFT. MBSR is also closely related to hypnosis and trance, and seeing a board-certified hypnotist can be beneficial in quickly countering negative beliefs held by your subconscious that can intensify feelings of physical pain. Clinicians trained in neuro-linguistic programming (NLP) can also be beneficial in this way. If CPP is related to trauma, EMDR (eye movement desensitization and reprocessing) may be a recommended modality of treatment as well.
Practitioners also might recommend a diet and nutritional program to follow, as there can be a demonstrated correlation between gut health and CPP symptoms. An anti-inflammatory diet is most often recommended for folks managing CPP.
Finally, a yoga and gentle stretching program can be beneficial for people managing CPP. Getting more in tune with your body, and learning ways to stretch, move, and strengthen muscles can give you a sense of control over your own body and pain. Working alongside an experienced yoga practitioner and a physical therapist may not only increase your knowledge about pain and anatomy, but give you tools you can take home to treat, stretch, and strengthen your own muscles.

How To Talk About Your Painful Pelvis
Talking with loved ones (and folks who are anything but!) can be likened to a “coming out” experience for people diagnosed with CPP. Coming out as a person managing a chronic condition can be scary, particularly if you feel uncomfortable or unsure discussing intimate details of your health with others. Many folks managing CPP that I have spoken with often feel afraid to tell others, or only share parts of their story, or discuss “back pain” with their families, partners, colleagues, and supervisors. That’s all normal. Your health journey is yours. You choose what to share with others. I do want to encourage you to bravely share what you like with others. I recognize women’s sexual health and anatomy is often stigmatized. I encourage you, where comfortable, to take your own vulvas and vaginas back, and to bravely exist as a person with genitals. That said,
Broaching the subject with family
- You may need to advocate for yourself with seating options, or length of time spent seated at family gatherings.
- You may need to discuss clothing for certain events in order to wear looser- fitting or more comfortable clothing.
- Understand that you might be managing others’ reactions to previously unknown or misunderstood medical conditions and female anatomy. Make space to lovingly educate others while also taking into account that you are not an encyclopedia and can only help so much. Set your own boundaries with these conversations and feel empowered to uphold them.
- Remember times that family gathered and talked about their “health stuff.” Use these examples to empower yourself in knowing that it is OK to discuss with others.
Coming out at work
- Set up a private meeting with your supervisor if you need to talk to them about accommodations such as chair options, seated/standing desks, wardrobe changes, etc.
- Define terms like neuropathic pain and pelvic floor dysfunction to help them better understand the physiology behind the condition.
- Explain what “treatment” looks like (managing symptoms vs “curing” them).
- Remember that you provide a benefit to your company or organization, and that it’s acceptable for you to take up space and need human accommodations as a person with a body.
Talking with a partner
- You may be feeling as though you aren’t a “complete” partner because you are “missing” something sexually, the ability to engage in certain genital touching or stimulation. Redefining what a relationship looks like and listing out all the other non-sexual parts of your relationship that matter can be beneficial.
- Consider asking yourself, if your partner was going through this, wouldn’t you want them to be open and honest about their experiences?
- Also consider asking yourself if you would have empathy for a partner struggling with a chronic condition or pain. Understand that your partner will likely also grant you that loving courtesy and consideration.
- If a partner reacts poorly, pressures you into sexual activity, or guilts and shames you, ask yourself if this is the kind of person you want to be with. Feel brave in communicating how your partner’s reactions affect you.
Adjusting Your Lifestyle
Listen to your body. Your body will tell you what is manageable in terms of sitting, standing, stretching, and what clothes are okay or not.

Many women with CPP report that wearing tight underwear and pants can exacerbate their pain. Some women find looser-fitting or seamless underwear that does not irritate them further, or just go without underwear entirely. It is totally acceptable to go commando. You might just have to wash your pants more often than usual, but there is nothing “not normal” about not wearing panties.
Women also search for clothing that helps to not constrict their pelvic floor. Jeans are often a culprit of painful tightness or ill-placed seams. It’s been recommended that the best styles of bottoms for people with CPP are loose-fitting “paper bag pants” or midi-skirts. Recommended brands include Target ($), Madewell ($$), Modcloth ($$), and Free People ($$$).
Some folks with CPP also choose to add cushioning to their seating to improve their pain. There are many different types of pillows and rings made for lower back pain or hemorrhoids (I know) that can help to alleviate pain with sitting.
For folks who have an established exercise routine or who go to the gym and are managing CPP, adjustments might need to be made. The best resource for information on this would be to refer to your physical therapist. Some people choose to use recumbent bikes, rather than upright bikes which can irritate or exacerbate pain in the vulvarvaginal area. Some exercises and stretches might be contraindicated as they might cause a flare-up or additional swelling or trauma to the pelvic floor muscles, such as by overworking the inner hip adductor. Regular loosening and warming-up exercises are encouraged before a workout, so as not to allow muscles to further seize up, which could potentially stagnate or reverse any progress you may be making.
Sex With CPP
(particularly for folks with vulvas who have a partner with a penis)
How about sex? When you’re dealing with CPP, “sex” can take on a whole new meaning. PIV (penis in vagina) intercourse can become stressful, pressuring, and painful. Managing CPP will likely mean that you have to change your sex life to accommodate your own experiences of pleasure, stress, pain, medical needs and recommendations, relationships, and communication. And that’s ok. The definition of sex we are given by society is rudimentary and inflexible. It doesn’t account for individual differences or for the reality that people have bodies that feel pleasure in different ways, and sometimes malfunction, among other things.
Expanding your definition of sex will be beneficial — for you, for your partners, for folks who don’t experience CPP, and honestly, for everyone. What does this mean? I recommend taking an inventory of, “What do I like?” What brings you pleasure, what turns you on, what makes you feel comfortable and safe and aroused and good? It’s ok if this has changed since your experiences with CPP. Sexual feelings and desires wax and wane with life events and changes. I encourage you to consider the positive sexual experiences you’ve had. What made those experiences good? Can you think of things that made you feel good outside of the traditional prescribed PIV stuff that society says you “should” want?
(Stay tuned for a write-up from me on no-goal sex, in the meantime, check out “Sex is not a performance”)
Maybe you get great pleasure from a hot shower with a partner. Maybe you really, really like making out. Maybe you like feeling the body weight of a partner on top of you. Maybe you like reading erotica. Whatever it is you find stokes the fire, great. You can practice with yourself or with partners.
I have found that a lot of folks with CPP feel that they “owe” a partner PIV sex. It’s how they were taught, directly, indirectly, or otherwise, how someone can be a good spouse, partner, girlfriend, friend with benefits, or what have you.
Let’s expand the definition of a good sexual experience! Let’s expand the definition of what makes you a good and valid human being!
You do not owe anyone sex.
You are not burdening someone by having to change your sex life to fit your physical needs.
Your body is valid and deserves to not endure increased stress and pain to accommodate another person.
You are allowed to decide and have autonomy over what your body does.
Say it with me please.
You do not need to have PIV sex to have a complete sexual experience.
You do not need to orgasm or bring a partner to orgasm to have a complete sexual experience.
You are allowed to communicate and speak up and change what is occurring during sex if you’d like to. For any reason.
You are allowed to say no.
You’re also allowed to say yes! To yourself, to what you would like sex to be, to things that interest and excite you, to your partner, to the experience you would like to have.
If your self-worth is tied into your sexuality, I am sorry. You are not alone. I’m here with you. Our society has really done a number on folks, us included. Let’s bravely work to entangle and deconstruct this, together.
You will find benefits to expanding your definition of sex. No-goal sex is great, pleasure-centered, and much less stressful.
However — it does require communication. You may be thankful to find that a sexual partner you are involved with has been doing this work. Or, you may have to bravely and gently guide them on expanding your definition of sex. You may be going on this journey solo and will benefit from communicating with yourself! 🙂 Whatever may be the case, practicing talking about sex will be very helpful. Practicing assertive communication is important to having satisfying sexual experiences, CPP or not.

How do we communicate about sex?
Great question.
Here are some resources I will guide you to —
In Come As You Are, Emily Nagoski recommends taking an inventory of good and not-so-good sexual experiences to inform your understanding of which things to seek out and which things to avoid. Knowing this can help you discover what you would like to communicate about and negotiate.
If conflict occurs, I highly recommend an imago method of communication, put forth by Harville Hendrix in his book, Getting the Love You Want. This is a slow and measured form of communication to ensure both partners feel heard. I highly recommend reading more on it. In her book, Getting the Sex You Want, Tammy Nelson took Hendrix’s imago therapy and specifically applied it to communication around sex and intimacy.
I will write more about these in the future I’m sure, but above is a rudimentary overview. Honestly, I feel the skills about the how in communication often pale in comparison to the when, which is sometimes tougher to access for folks who are inexperienced in communication or feel afraid, guilty, ashamed, or self-conscious. Overcoming your own barriers to sexual communication is a more important and immediate goalpost to focus on when you are managing CPP. I encourage you to seek therapy, practice mindfulness, learn more about your sexual self, and practice, practice, practice.
For the nuts and bolts of sex, talk to your physical therapist about recommendations specific to you, your anatomy, and your pain. Some women find relief when using products such as the ohnut, which can help to lessen the pain with deeper penetration when having PIV sex with a partner. As previously mentioned, lube can be a godsend. There are certain sexual positions that might be better than others. And, it will likely be recommended by a physical therapist that you pick up a set of quality dilators.
Recommended Reading:

Better Sex Through Mindfulness
Read My Lips: A Complete Guide to the Vagina and Vulva
The Return of Desire: A Guide to Rediscovering Your Sexual Passion
Secret Suffering: How Women’s Sexual and Pelvic Pain Affects Their Relationships
Sex for One: The Joy of Selfloving
Women Who Love Sex: Ordinary Women Describe Their Paths to Pleasure, Intimacy, and Ecstasy
This article was written in cooperation with my colleague and fellow sexual empowerment activist, Kathleen. Thanks for your help!
Any questions or further suggestions for this resource? Please email me.